Pelvic organ prolapse: Understanding anatomy does make a difference
Vaginal wall prolapse repair requires an in-depth understanding of the three most common pathological mechanisms.
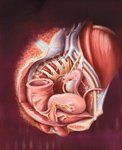
Our goals here are to review the anatomy of the posterior compartment and to describe three types of posterior wall failure: (1) failure that's distal in the perineal body (2) failure of the levator ani muscles to close the genital hiatus, and (3) failure that's more proximal with the loss of upward suspension of the posterior wall by the uterosacral ligaments. Clinically, loss of support at any of these levels results in the formation of a rectocele with or without an enterocele and perineocele. The surgical correction of the posterior wall can be tailored by specifically approaching the underlying mechanistic defect, in an attempt to restore normal anatomic support.
Understanding the anatomy

The upper suspension of the posterior vaginal wall (top of the container) is created by its attachment to the uterosacral ligaments, which extend below the peritoneum and can be seen in MRI imaging.5 All of these boundaries are subject to defects that can give rise to different structural failures.
Where do posterior wall failures occur?

Buprenorphine use in pregnancy linked to decreased fetal breathing movements
May 18th 2024According to a poster presented at ACOG 2024, use of the synthetic opioid buprenorphine depressed fetal breathing in biophysical profile assessments, but had no significant impact on other factors like amniotic fluid index or fetal tone.
Read More
Laparoscopic RFA linked to enhanced pregnancy outcomes in uterine fibroid patients
May 18th 2024A recent study presented at the 2024 ACOG Clinical and Scientific Meeting reveals that laparoscopic radiofrequency ablation significantly improves pregnancy outcomes for women with uterine leiomyomas.
Read More
Identifying gaps in syphilis treatment and prenatal care among pregnant individuals
May 17th 2024Preventing congenital syphilis comes down to quick diagnosis and treatment of the infection in pregnancy, and the number of missed opportunities to do so in the United States continues to grow.
Read More
